Navigating the Medicare Landscape: Understanding the MAC Program
Related Articles: Navigating the Medicare Landscape: Understanding the MAC Program
Introduction
With great pleasure, we will explore the intriguing topic related to Navigating the Medicare Landscape: Understanding the MAC Program. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
- 1 Related Articles: Navigating the Medicare Landscape: Understanding the MAC Program
- 2 Introduction
- 3 Navigating the Medicare Landscape: Understanding the MAC Program
- 3.1 Understanding the Role of MACs in Medicare
- 3.2 The Importance of MACs in Ensuring Program Integrity
- 3.3 Navigating the MAC Program: Key Considerations
- 3.4 Frequently Asked Questions (FAQs) About the MAC Program
- 3.5 Tips for Navigating the MAC Program
- 3.6 Conclusion
- 4 Closure
Navigating the Medicare Landscape: Understanding the MAC Program

The Medicare program, a vital component of the American healthcare system, provides health insurance coverage to millions of individuals aged 65 and older, as well as younger individuals with disabilities. While the program is vast and complex, its administration is streamlined through a network of regional contractors known as Medicare Administrative Contractors (MACs). These contractors play a crucial role in ensuring the efficient and effective operation of Medicare, particularly when it comes to processing claims and ensuring compliance with program rules.
Understanding the Role of MACs in Medicare
MACs are private entities contracted by the Centers for Medicare & Medicaid Services (CMS) to administer Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) in specific geographic regions. They are responsible for a wide range of tasks, including:
- Processing claims: MACs receive and process claims submitted by healthcare providers for services rendered to Medicare beneficiaries. They ensure the claims are accurate, compliant with program rules, and eligible for reimbursement.
- Provider enrollment and credentialing: MACs manage the enrollment and credentialing process for healthcare providers who wish to participate in the Medicare program. This involves verifying the provider’s qualifications and ensuring they meet the program’s requirements.
- Provider education and outreach: MACs conduct educational programs and outreach initiatives to inform providers about Medicare program rules, regulations, and best practices. This helps ensure providers are compliant and can effectively serve Medicare beneficiaries.
- Fraud and abuse detection: MACs play a critical role in detecting and preventing fraud, waste, and abuse within the Medicare program. They investigate suspicious claims and work with law enforcement agencies to pursue criminal activity.
- Beneficiary outreach and support: MACs provide information and support to Medicare beneficiaries, helping them understand their coverage, access benefits, and navigate the program.
The Importance of MACs in Ensuring Program Integrity
MACs are essential to the integrity and efficiency of the Medicare program. They act as a vital link between CMS and healthcare providers, ensuring that claims are processed accurately and that providers are compliant with program rules. This helps to prevent unnecessary costs, protect beneficiaries from fraud, and ensure the program’s sustainability.
Navigating the MAC Program: Key Considerations
Navigating the Medicare program can be challenging for both healthcare providers and beneficiaries. Understanding the role of MACs and their specific responsibilities within each region is crucial for navigating the program effectively.
Here are some key considerations for healthcare providers:
- Provider enrollment and credentialing: Healthcare providers who wish to participate in the Medicare program must go through a rigorous enrollment and credentialing process. This involves submitting documentation, undergoing background checks, and meeting specific requirements. MACs are responsible for managing this process, ensuring that only qualified providers can participate in the program.
- Claim submission and processing: Healthcare providers must submit claims for services rendered to Medicare beneficiaries through the appropriate MAC. It is essential to understand the specific requirements and deadlines for claim submission, as well as the procedures for appealing denied claims.
- Staying informed about program changes: The Medicare program is constantly evolving, with new rules and regulations being implemented regularly. It is crucial for providers to stay informed about these changes and to understand how they impact their practice. MACs provide resources and educational programs to help providers stay up-to-date.
- Compliance with program rules: Healthcare providers must adhere to all Medicare program rules and regulations. MACs provide guidance and resources to help providers understand these rules and ensure compliance. Failure to comply can result in penalties or sanctions.
Here are some key considerations for beneficiaries:
- Understanding your coverage: Medicare beneficiaries should understand the scope of their coverage, including the benefits they are entitled to and the costs they are responsible for. MACs can provide information and support to help beneficiaries understand their coverage and navigate the program.
- Accessing benefits: Beneficiaries should know how to access their benefits, including how to find healthcare providers who accept Medicare, how to file claims, and how to appeal denied claims. MACs can provide guidance and support in these areas.
- Staying informed about program changes: Beneficiaries should be aware of any changes to the Medicare program that could affect their coverage or benefits. MACs provide resources and information to help beneficiaries stay informed.
- Reporting fraud and abuse: If beneficiaries suspect fraud or abuse within the Medicare program, they should report it to the appropriate authorities. MACs have dedicated fraud and abuse units that investigate these reports.
Frequently Asked Questions (FAQs) About the MAC Program
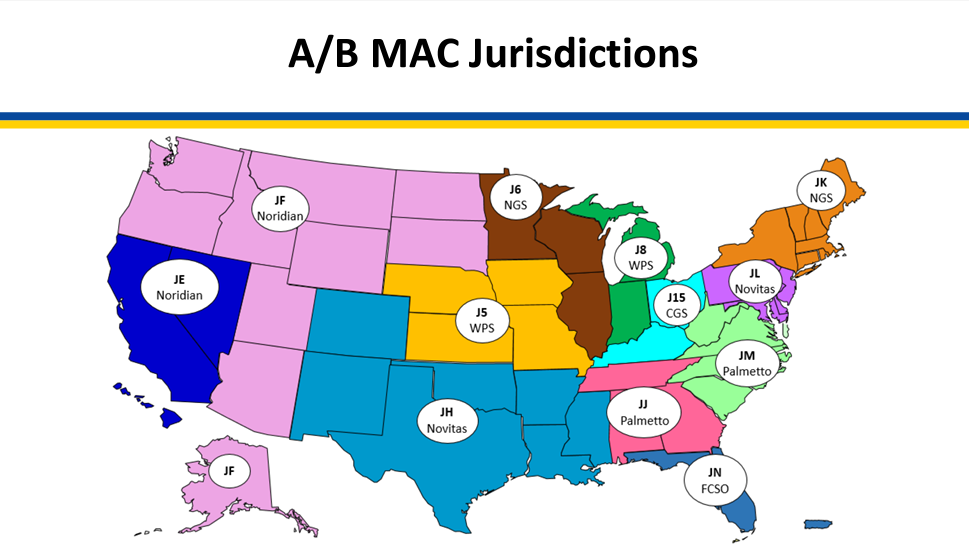
Q: How do I find the MAC responsible for my region?
A: The CMS website provides a map that outlines the geographic regions covered by each MAC. You can also contact CMS directly for assistance in identifying your MAC.
Q: What are the different types of MACs?
A: There are two types of MACs:
- A/B MACs: These MACs are responsible for administering both Medicare Part A and Part B.
- DME MACs: These MACs are responsible for administering Medicare Part B claims for durable medical equipment (DME), prosthetics, orthotics, and supplies.
Q: How do I contact my MAC?
A: Each MAC has a website and a dedicated phone number for beneficiary and provider inquiries. You can find this information on the CMS website or through a simple online search.
Q: What are the benefits of working with a MAC?
A: Working with a MAC offers numerous benefits, including:
- Efficient claim processing: MACs streamline the claim processing process, ensuring timely and accurate reimbursements.
- Compliance support: MACs provide guidance and resources to help providers comply with Medicare program rules and regulations.
- Fraud and abuse prevention: MACs play a vital role in detecting and preventing fraud, waste, and abuse within the Medicare program.
- Beneficiary outreach and support: MACs provide information and support to Medicare beneficiaries, helping them understand their coverage and access benefits.
Tips for Navigating the MAC Program
For healthcare providers:
- Stay up-to-date on program changes: Regularly review CMS updates and announcements regarding Medicare program rules and regulations.
- Utilize MAC resources: Take advantage of the educational materials and resources provided by your MAC, including online training modules, webinars, and publications.
- Develop a strong compliance program: Implement robust policies and procedures to ensure your practice is compliant with Medicare program rules.
- Maintain accurate records: Keep detailed records of all services rendered to Medicare beneficiaries, including dates of service, diagnosis codes, and treatment plans.
- Submit claims accurately and timely: Ensure that all claims are submitted with accurate information and within the designated deadlines.
- Appeal denied claims: If a claim is denied, understand the appeals process and file an appeal within the specified timeframe.
For beneficiaries:
- Understand your Medicare benefits: Review your Medicare summary of benefits and understand the coverage you have.
- Find a provider who accepts Medicare: Use the Medicare provider directory to locate healthcare providers who accept Medicare.
- Keep track of your medical records: Maintain copies of your medical records and keep them organized.
- Ask questions: Don’t hesitate to ask questions if you are unsure about anything related to your Medicare coverage or benefits.
- Report fraud and abuse: If you suspect fraud or abuse within the Medicare program, report it to the appropriate authorities.
Conclusion
The Medicare Administrative Contractor (MAC) program is a vital part of the Medicare system, ensuring the efficient and effective administration of the program across various geographic regions. By understanding the role of MACs and their specific responsibilities, both healthcare providers and beneficiaries can navigate the Medicare landscape more effectively, ensuring access to essential healthcare services and protecting the integrity of the program. As the Medicare program continues to evolve, the role of MACs will remain crucial in ensuring its continued success and providing vital healthcare services to millions of Americans.
![Navigating Medicare [INFOGRAPHIC]](https://www.thenoblegroup.com/-/media/rj/common/resources/retirement/navigating-medicare-2023-1.png)




Closure
Thus, we hope this article has provided valuable insights into Navigating the Medicare Landscape: Understanding the MAC Program. We appreciate your attention to our article. See you in our next article!